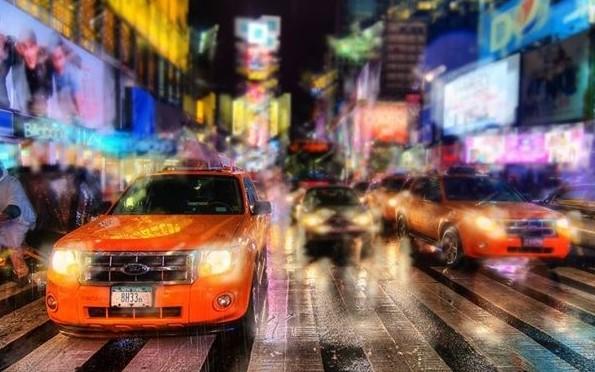
Is this how you see the world?
Keratoconus is:
- frustrating because glasses and regular contact lenses don’t give clear vision, and the world looks like what you see in the image above.
- a progressive, degenerative disorder.
- characterised by thinning and bulging of the cornea.
- a type of corneal ectasia.
Treatment options:
- Glasses or soft contact lenses
- Complex contact lenses
- Collagen cross-linking
- Corneal ring segments
- Corneal transplant (keratoplasty)
Corneal Ectasia
This process of thinning and re-shaping of the cornea is called corneal ectasia.
Keratoconus is just one of many types of corneal ectasia.
The cornea is the clear, front surface of the eye and it helps to focus light onto the retina. Any distortion of the cornea leads to blurred vision, and the more advanced the keratoconus, the more blurred the vision will be.
The real cause of keratoconus is unfortunately not fully understood, but it appears that there may be a genetic component and it’s believed that rubbing the cornea can speed up the degeneration. So controlling the itch that makes one want to rub one’s eyes is key in any keratoconus management plan. Usually keratoconus progresses faster in younger eyes, so it’s important we find these cases early in life, and treat them as soon as possible.Treatment options explained:
Control the itch
Do everything possible to reduce itchy eyes:
- Avoid the things that irritate your eyes.
- Wear sunglasses, glasses or goggles to shield your eyes.
- Use regular eye lubricant drops hourly to flush out pollens/irritants before they build up.
- Tightly squeeze your eyelids shut to secrete more oil to lubricate your eyes.
- Use cold ice-packs to soothe swollen eyelids and reduce the itchiness.
- Use eye drops such as Zaditen and Patanol as recommended by your optometrist.
- DON’T RUB YOUR EYES.
Glasses or soft contact lenses
In early keratoconus, the best treatment is to sharpen the vision with prescription glasses or soft contact lenses. Neither do anything to slow the changes to the cornea because the progression at this stage is either non-existent or so mild it’s not worth the hassle or expense of the options listed below.
Complex contact lenses
When soft lenses can no longer give clear vision, we have several options to choose from – rigid gas permeable (RGP), hybrid or scleral lenses. These are custom made for your eyes, from gas permeable materials, masking the abnormal shape of the cornea, and sharpening your vision.
Collagen cross-linking (CXL)
We recommend all keratoconics in their teens or 20s see an ophthalmologist as soon as possible in case CXL can stabilise the corneas at a time when the corneas are likely to progress the most.
CXL strengthens the cornea by applying collagen and riboflavin (vitamin B2) to the cornea.
There are 2 options, with the front layer/epithelium either left intact or removed, before the cornea is saturated with the solution and UV light applied, bonding the collagen strands into a meshwork that strengthens the cornea. Early treatment with collagen cross-linking can slow or even stop the progression of keratoconus.
CXL takes about an hour and is performed by an ophthalmologist, who will review months later, and advise when the eyes are stable and ready to be fitted with contact lenses.
Corneal ring segments
This is a surgical option involving the insertion of clear plastic segments into the cornea. These segments are designed to reshape the front surface of the eye, thus correcting refractive errors caused by keratoconus. Corneal ring segments are reserved for advanced cases of corneal ectasia, where the patient’s vision is not correctable with glasses or contact lenses.Corneal transplantation (keratoplasty)This is an option only if all other treatments have been tried or ruled out. Fortunately, only 10–20% of keratoconic eyes eventually require corneal transplantation.
There are two types of corneal transplants – partial-thickness and full-thickness – and it is usually the latter that is recommended for patients with keratoconus.
A corneal transplant is a complex procedure but is only day surgery. It is usually performed under local anaesthetic, with the option of a sedative. During the procedure, your surgeon will cut out the abnormal section of cornea and replace it with donor cornea, which will be stitched into place. The stitches will be removed at a later date. Your own corneal cells will gradually grow around and fuse to the implanted cornea, and a full recovery might take up to a year.
Crosslinking cannot be performed on patients:
- if their cornea is too thin (generally less than 350-400 microns)
- with an active ocular disease other than keratoconus
- with herpes simplex keratitis, a corneal infection caused by the herpes simplex virus (cold sore)
- who are pregnant
- with active, uncontrolled eye allergies
- with corneal scarring that significantly affects their vision
FAQs
Are contact lenses for everyone?
The short answer is no, but most patients can wear them and one of our optometrists will check your eyes and let you know if you are suitable for contact lenses. When the vision with glasses is poor in one eye but good in the other, some people choose to not correct the poor vision but if they are keen to play sport at a high level, their depth perception is very important and they will choose to correct both eyes.
Am I really allergic to rigid contact lenses?
Usually not – it’s usually the contact lens solution or the fit of the lens that causes the issues. The success rate for RGPs amongst keratoconus patients is around 85%. Most allergic reactions or rigid lens failures or rigid lens dropouts arise from poor contact lens fits by inexperienced practitioners.
The only alternative to rigid contact lenses for most people with keratoconus is surgery – notably corneal transplantation – so it is worthwhile finding a specialist contact lens fitter for keratoconus.
Can wearing contact lenses cure my keratoconus by reshaping my cornea?
No. RGPs and scleral lenses improve vision by covering the irregular cornea but they don’t remould the cornea – and they most definitely shouldn’t because rubbing the surface of the eye can induce scarring and cause great discomfort while wearing the lens.
Can wearing contact lenses make my keratoconus worse?
Only if the lens fits badly and rubs the cornea as described in the question immediately above.
Is it safe to sleep in my contact lenses?
Absolutely not. I can’t be more stringent on this topic. Someone who has to wear RGPs or scleral lenses has a compromised cornea, and sleeping with the lenses on the eye deprives the cornea of oxygen, and the combination of those 2 factors never ends well. Low oxygen levels means cells die off, which leads to a sharp increase in the risk of serious eye infections, permanent scarring and, in the worst cases, a loss of vision or blindness. It’s always best to remove the lenses before you sleep, even for a short afternoon nap, and reinsert afterwards – of course, this means storing the lenses in conditioning solution and not leaving them to dry out.
What if I fall asleep while wearing my lenses?
Don’t remove the lenses right away but rather put a few drops of eye lubricant or saline in your eyes, massage the lenses through your closed lids, and press the edge of the lower lid beneath the bottom edge of the lens to break the seal of the lens against the eye. Only then should you try to remove the lens with a plunger. If your eyes are red or irritated 30 minutes after removing the lenses, come in to see your optometrist – we’ll check if your cornea is healthy and ready to wear a lens again. It’s important to stop wearing lenses if your eye is RED, SORE or BLURRY (your vision is blurry).